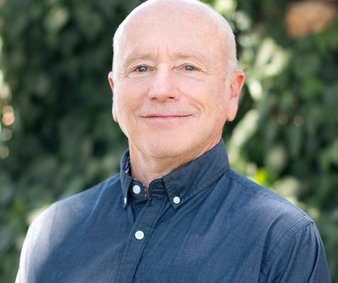
As cases of COVID-19 surge with the spread of the Omicron variant, local health officials are working together to help communities stay healthy. Stanislaus County Public Health Officer Dr. Julie Vaishampayan and Emanuel Medical Center CEO Dr. Murali Naidu talked with the Journal about how Omicron is different than other COVID-19 variants, the impact surging cases are having on Turlock’s hospital and how residents can help prevent severe illness.
Journal: How is the Omicron variant different from the first strain of COVID-19?
Dr. Vaishampayan: I think you are pretty well aware that Omicron emerged sometime in November, and rapidly took over in the world overtaking Delta as the predominant strain circulating. Omicron has a growth advantage, and this growth advantage makes it a little bit easier to spread from person to person, but a large part of it is due to its ability to evade the immune system. Any immunity that they have from one or two doses of vaccine or a previous infection, the virus is still able to cause infection. So this evasion of the immune system has definitely given it an advantage to take over and spread quite widely for the severity.
If you look over the population, it is definitely less severe. However, if it would be an infection of any one person that has no previous immunity from like, say vaccine or previous infection, and so you look at that, compared to say Delta or one of the others, is it less severe when you do that comparison? I think that's really hard to say. I think there are some emerging data now that yes, it does seem to be overall less severe. But I think there's more to come on that one. So that's a little bit difficult. But the main problem we've been struggling with, of course, is its growth advantage and immune evasion…This immune evasion has caused some problems in the people who are fully vaccinated who can still get it. A booster does raise the level of immunity some, so it makes it less likely to be infected. So that's good. I think it brings it up to about 70% protection. So a booster is a good thing to go get, being fully vaccinated and boosted. And I'm just talking about for infection right now.
And another thing that has been a problem is some of the treatments available, the monoclonal antibodies, we lost two of our three monoclonal antibodies, because they no longer had potency. They didn't work for this variant to the virus. And so we were down to just one of our three treatment monoclonal antibodies. So that has been an ongoing struggle is that one that was left is the one that was in the shortest supply.
As we look at hospitalizations and deaths, what we call severe disease, what we have seen is that vaccination is definitely protective and it's maintained its protection in hospitalization and severe disease. We do know from Delta that previous infection also prevented against severe disease, but we have not yet seen data from Omicron. So even if you get infected after your vaccination with Omicron, you are highly protected against severe disease and death. And then the booster adds some additional protection. It's about 80% protected for a fully vaccinated person, and then adding that booster gets it up to the 90%. That’s really good news that the vaccine has maintained that protection against severe disease
Journal: What kind of impact has Omicron, and the entire COVID-19 pandemic, had on the general public health?
Dr. Vaishampayan: I think in overcoming all of the COVID-19 variants one of the biggest problems has been it causing severe disease with people who have previous medical diagnosis. So people with diabetes with heart disease with lung disease, and it's really had pretty severe impact on people who are older as well, certainly greater than 65. Those greater than 50 also are in the risk increasing with age and it's really hit people hard that already have some underlying diseases, and that includes being obese — the underlying disease that hits all age groups as well…We've seen this become the number three cause of death in the United States. You certainly see that getting the top five causes of death for children. It certainly has had an impact on mortality in the United States, in California and Stanislaus County.
There is also this long COVID, which means that people can have symptoms that linger for weeks to months afterwards and is still being defined of what that is. But what has become clear is that this is going to impact health ongoing for many people as they recover from infections.
Journal: With COVID-19, it feels like this is the first time the public has been aware of medical professionals trying to create disease prevention and treatment as a disease emerges. As a public health expert, is this something you deal with a lot or is this something truly historic?
Dr. Vaishampayan: This is something truly historic. There have been other emerging diseases, but they don't tend to hit the whole population all at once. You think of West Nile virus and it took it years to just roll across the United States. And so, by the time it hit California there had been many years of data from the East Coast. And it doesn't seem to hit the whole population. You think of the Hantavirus that emerged in the Four Corners area, but that has a specific rodent exposure. So, for one that hits and affects everybody at the same time, when there's so much learning that needs to be done, I would say this is pretty unique in the quickness and the changing of the information and the fact that the information has had to change along with the virus because what you knew of one variant didn't necessarily hold out as much as the next one. The incubation period has shortened — that's the time from when someone is exposed and gets infected to when they have symptoms and they are passing it on to someone else. It started out at five days and it went on for days and now it’s two to three days. I mean, I've seen figures as low as 42 hours at this point. So the virus has been changing and we just learned as fast as the last barrier and it feels like it's really been a struggle to keep up and keep knowledge flowing. I can't think of a time when this has happened before.
Journal: How is COVID-19 different than the seasonal flu?
Dr. Vaishampayan: I would say at this point, it’s still appearing to be more severe than the flu. When it first came out, it was certainly a severe disease. And with Omicron, I think it's getting closer to look like what we see with a seasonal flu, but it's still I would say more severe. In Omicron especially, it has come to be the same if we look at spreading before people developed symptoms and the way in which spreads, which is both droplet and airborne – and there's been tons of arguments about that. It's clearly both. Some of the ways that it's very different is we don't have the treatments available yet. I mean, you can present to your doctor with flu like symptoms before this pandemic and they could just give you a prescription for Tamiflu, and you can go on your way, right? We didn't have that available. We're still not quite at that point yet. So the treatments are not available yet that we can go down to treating this like a flu. Then, of course, when it came out, there was no immunity in the population and we're not used to everybody being susceptible to a virus. There’s always some level of immunity, either from vaccine or you've seen this one before and had it last year. Just having a fully susceptible population really made the spread and severity so much worse. I think it's getting closer (to being more like seasonal flu) at this time, but we still have a little bit of ways to go, especially the treatment regimens and availability.
Dr. Naidu: There isn't some level of natural immunity, like there has been for other diseases that have come through. When it’s really impacting so much of the population and for us and the other hospitals that’s including our health care workers. So, it's really a challenge when we've got the risk of people getting sick with something that's actually quite a bit more transmissible than the flu and pulling our healthcare workers away when the hospital is still full. And that's a big challenge for every hospital in the country and world I would go as far as to say.
Journal: How has the Omicron surge impacted Emanuel Medical Center?
Dr. Naidu: Our ED (Emergency Department) is easily the most impacted by the Omicron strain. And what we've seen is because of that increased transmissibility that Dr. Vaishampayan mentioned, it really has spread more quickly than even any other part of the pandemic. That has brought people into the emergency room in some cases for testing alone, because at the same time, people are trying to get their kids back in school and so forth and so on. And then add in that we're in the midst of the cold season and coming off the holidays. All of that really impacts the emergency department across the county. I've had the opportunity to connect with my colleagues at the other hospitals and we're all seeing this so that higher volume of people coming to the ED has been a pretty big impact during this specific Omicron driven wave.
The other side of that is the disease isn't as severe at some of the other variants we've seen. And so the percent of those individuals that need to be hospitalized is lower, however, because so many more people came into the ER all of our hospitals in the county have had still very high numbers of admissions for COVID. We actually got up to our previous peak a little bit earlier in the month —and that's true, again, at the other hospitals. We all kind of got there around the same time. We've now come down a bit and are holding steady, but we're not back down to a low level. We're just a little bit lower. And then lastly, I'll say about severe disease. We're seeing a lower percentage of those patients subsequently needing the intensive care unit. Again lots of absolute numbers, but the percent requiring the intensive care unit has been lower.
Journal: Final thoughts?
Dr. Naidu: For me coming into the community as a new hospital leader, I want to just express my thanks to Dr. Vaishampayan. I don't know if the community at large appreciates how valuable it is to have an infectious disease physician as their public health officer, especially during a pandemic, but it's really something that for Stanislaus County generally and certainly for us here in Turlock is tremendously valuable.
Dr. Vaishampayan: I have to say that the hospitals, all of them, including the leadership of Emanuel, have been absolutely the best partners. Throughout this pandemic, we’ve been working together closely trying to ensure that everything works together from when someone hits the emergency department to how to care for them after discharge… We’re establishing relationships that I think are going to carry us into the future and really help improve all care in the county and health in the county.
You know, public health is about prevention, right? We're about raising the health of the entire population. And we like to prevent disease. We'd like to prevent diabetes by working on healthy, eating active living, promoting fruits and vegetables and sharing those access to the community. So as we look at COVID and trying to prevent disease with this vaccination is just really our most key prevention. While it might not stop you from getting sick, it's going to stop you from needing hospital care. It can prevent bad outcomes, such as death.
There are also treatments that are available in our community. So if someone does test positive and are at risk for severe disease, there are treatments available and we really want to promote people talking to their health care provider to ensure that they can access these treatments.